Introduction
Editor’s Note: On April 5, 2022, CMS released a FAQ on Good Faith Estimates. Two issues were clarified and have changed in this article: 1) GFEs are not required for appointments made within 3 days, 2) GFE’s are a part of a patient’s full medical record. Those changes are reflected below.
The No Surprises Act was passed at the end of 2020 as a part of the Consolidated Appropriations Act of 2021. Initially most experts believed that the No Surprises Act applied only to facility-based (such as hospital) providers; however, on the recent finalization of Part II of the rules, it became clearer that a specific portion applies to all health care providers.
One of the new No Surprises Act’s major goals is to ensure that patients do not receive health care bills that far exceed their awareness or expectations. Although the most heralded portions of the law (usually pertaining to hospital services) do not apply to the vast majority of chiropractic physicians, another key provision pertaining to “good faith estimates” will apply to nearly all chiropractic offices beginning on January 1, 2022. Health and Human Services (HHS) issued rules, FAQs, and other information pertaining to the No Surprises Act throughout late 2021.
Through our coalition of state associations, the Alaska Chiropractic Society has continued to review and decipher the new available information from law and rules as it has and continues to evolve and make the information available to our members.
The No Surprises is comprised of two major parts. Part I is entitled: “Requirements Related to Air Ambulance Services, Agent and Broker Disclosures, and Provider Enforcement,” and Part II is “Requirements Related to Surprise Billing; Part II.” For reasons explained below, only Part II will apply to most chiropractic physicians.
Part I applies specifically to certain Medicare defined “facilities,” so it does not pertain to chiropractic physicians working in an office setting. “Facilities” include a hospital setting, a Federally Qualified Health Center, or another type of defined facility. At this time, offices that treat Medicare patients are not included in the definition of “facility”. Part I puts restrictions on air ambulance services and surprise billings from non-participating provider services in participating facilities (for example, an out-of-network anesthesiologist who provides services during surgery as part of a team of providers) and emergency service billings.
Part II, however, has a much broader application that does include chiropractic physicians. Its primary purpose is to better inform patients regarding the cost of care and require a “Good Faith Estimate.” Fortunately, the law limited the scope of this requirement to particular situations; however, it will still require all chiropractic physicians, whether insurance based, in-network, out of network, or cash, to make an initial determination for all patients whether a good faith estimate is required.
Although the No Surprises Act requires Good Faith Estimates (GFE) for both self-pay and insurance-based patients, HHS only issued rules for the patients who are uninsured or self-pay patients (see more information below). However, HHS is specifically excluding insured patients from current requirements (and enforcement) because the infrastructure is not available to provide meaningful information to the patient. This article will focus on the GFE requirements for uninsured or self-pay patients (Important: see below for definitions of “uninsured” and “self-pay.”).
Important Note: This regulation will impact your office in some way, since the minimum requirements will include required questions of patients, posters in your office, additions to your website, and paperwork for Medicare patients.
The information in this article is based on the Interim Final Rule that was active on October 7, 2021, but is subject to change because it is still in the comment period. Additionally, these interpretations are based on the best information currently available. Some of these requirements MAY change from future updates to the rule or based on court rulings. Nonetheless, these requirements are in place and active beginning January 1, 2022. Patients will be fully aware of these rights since the requirements will be in place for all healthcare providers. As the ACS receives more information, we will update this article and inform our members of the changes.
What are Good Faith Estimates (GFEs)
One of the key concepts of the No Surprises Act is to ensure that patients do not receive medical bills that are greater than they anticipate. Although the vast majority of the law focuses on large surprises from air ambulance and non-participating physicians at participating hospitals, they also want patients to know in advance the cost of services being rendered in non-emergency settings.
The law goes a step further than simply requiring a price list of services offered in the practice. Instead, providers must provide during scheduling (or before scheduling, if the patient requests) a clear list of services (with prices) anticipated for the specific patient.
Good Faith Estimates (or GFEs) have required elements:
- A list of all reasonably expected services for the scheduled visit with all prices,
- CPT codes and ICD-10 codes,
- Patient and provider identifying information,
- Appointment date (if scheduled), and
- Several disclaimers.
A full listing of required elements and an editable template are below in the GFE Required Elements and Form section.
Providers must present the Good Faith Estimate in writing, but they can also present it orally. HHS has clarified that providers can satisfy the written requirement through electronic means, such as email (if requested) or a patient portal. However, they clarify that the patient MUST have the ability to “both save and print” the GFE.
Who Is Entitled to Receive a GFE?
As mentioned above, the law includes all patients. However, the infrastructure is not available to provide this information to health insurance-based patients. Therefore, currently, only uninsured or self-pay patients will be entitled to a GFE.
The rules define uninsured (or self-pay) individual to mean an individual who does not have benefits for an item or service through their health insurance. In short, a “self-pay” individual:
- Does not have health insurance, OR
- Has health insurance, but is not billing the services being considered, OR
- Has health insurance, but does NOT have coverage for the services being considered (i.e. has Medicare, but needs and exam, x-rays, modalities, or therapies from a chiropractic physician). This will only apply if providers know the person does not have coverage for the services and items being considered.
Note that under bullet point 2 above, an individual with a high deductible plan who counts payment for the service toward their deductible would not be self-pay; however, an individual with a high deductible plan who declines to apply their out-of-pocket payment to their deductible is self-pay.
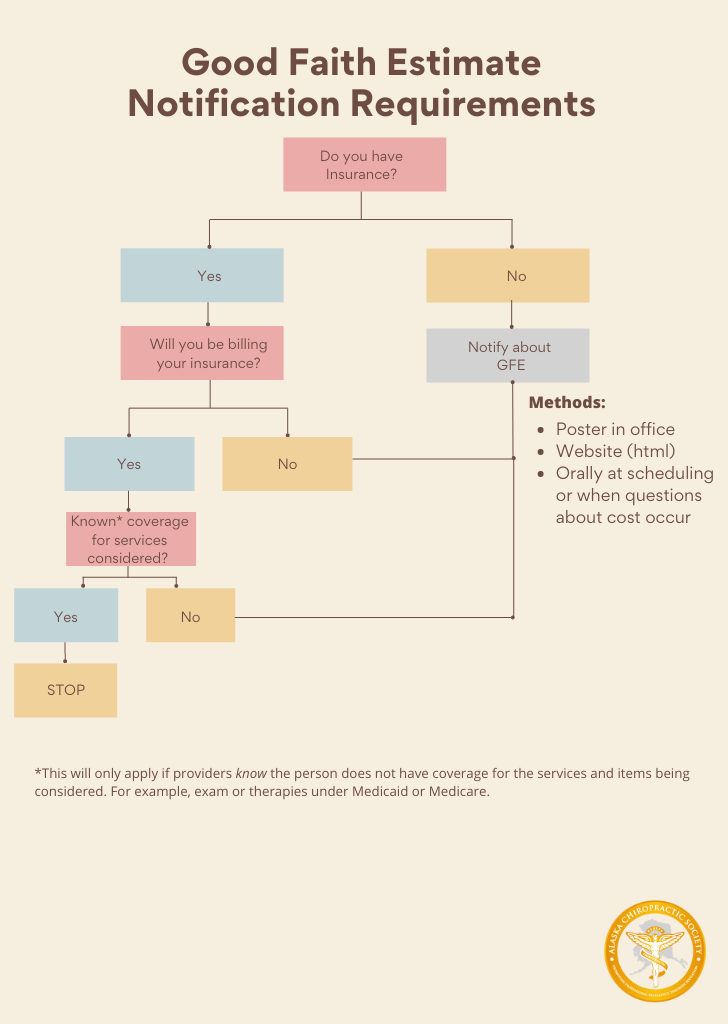
The staff person making the appointment is required to inquire about the information in all of the bullet points above, and, if the patient is a self-pay individual, notify them about the GFE (see “How Will Patients Know About the GFEs?” Section).
Important Note About Medicare: Since the rules requirement includes “an individual who does not have benefits for an item or service under a” health insurance plan (including Medicare), the ACS believes providers will have to provide a GFE to Medicare patients for exams, modalities, and therapies.
How Will Patients Know About the GFEs?
HHS requires providers to inform patients of their rights to receive or request a Good Faith Estimate. As a result, providers are required to notify patients in three specific, clear, and understandable ways:
- A notice prominently displayed in the office where patients can see the posting (download),
- A notice prominently displayed (and easily searchable from a public search engine) on your website (download), and
- Orally when a patient schedules an item or service or when questions about costs occurs.
Health care offices must provide all three types of notices. HHS has developed a template posting for the in-office posters. You can download that form here.
Additionally, you can use the same language in your website posting. However, do not simply upload the pdf to your website. Instead, you should make sure the language is in html format. This will ensure the “easily searchable from a public search engine” requirement is met. Click here to download a Word document with the HHS developed language.
Please remember that the rules require providers to notify self-pay patients that they are entitled to a Good Faith Estimate.
How to Implement the New GFE Requirements
These are examples of when a provider must give a GFE to patients.
Example 1: Patient calls to schedule an appointment for a new injury (no treatment plan)
When a patient calls to schedule an appointment for a new injury and no treatment plan is yet in place (i.e. no Good Faith Estimate already exists), then the staff member taking the appointment must take specific steps at the time the appointment is being made:
- Ask patients if they have health insurance and for the name of their insurance carrier/plan.
- If patients have health insurance, then ask if they intend to bill health insurance for the services.
- If the patient does not have insurance, does not intend to bill insurance, or does not have coverage for the intended item or service (i.e., examination and therapies for a Medicare patient), then the patient should be notified that they have the right to receive a Good Faith Estimate (see Required GFE Notifications section above).
- Best Practice – Notify the patient on the phone of the expected charges for their appointment. This will satisfy the oral requirements of the law. For example, if you typically perform an exam, x-rays, and adjustment on the first visit, then tell the patient, “Since this is a new injury, the doctor will perform an examination, may also need to take x-rays, and may perform an adjustment to treat your problem. That means that your first visit will cost between [exam cost] to [exam, x-rays, and adjustment cost]. We have this information in writing available to you, and you can pick it up anytime, including on the day of your visit.”
- Complete the GFE form and place it in the patient’s file.
When the patient arrives and requests a copy, simply make and provide a copy of the GFE form already in their file.
Example 2: After the doctor determines a treatment plan to patient
When the doctor determines the proper course of treatment and presents the plan to the patient (i.e., report of findings), this is the appropriate time to also present the patient with a Good Faith Estimate.
Although many of our doctors already require patients to sign a financial policy and other forms when patients are presented with treatment plans, for self-pay and uninsured patients, doctors will also have to present a form with the required GFE elements
When is the Good Faith Estimate Given to Patient?
The deadline for giving a patient the Good Faith Estimate (GFE) is based on when the patient makes a request, or schedules an appointment. Use this list that is based on the date an appointment is scheduled (in business days):
- 10 Days in Advance – Provide GFE 3 business days after the date of scheduling, or
- 3 – 9 Days in Advance – Provide GFE 1 business day after the date of scheduling, or
- Under 3 Days in Advance* – GFE is required if requested, or
- No appointment scheduled – Provide GFE 3 business days after the date the patient requests the GFE.* Note: Currently, experts are divided on interpreting whether or not a GFE is required at all if the appointment is scheduled less than 3 business days before the appointment time. However, because no court or agency has specifically ruled on this issue, prudent practice points toward providing a GFE when requested in these situations. Other Services Provided by Outside Entities (i.e., lab work)Interestingly, the rule requires that providers initiating the appointment gather fee information from other potential providers (called co-providers) that will bill patients directly. Although this requirement will most impact providers in hospital settings, the requirement applies to chiropractic physician offices, as well.The most common types of co-providers situations in chiropractic physician offices would be labs (typically functional medicine), radiologist readings, and physical therapy (independent PTs). As a physician, you will need to use your professional judgment to make the best determination regarding what types of potential co-providers might be needed for a particular patient.The rules require that the “provider or facility contact all applicable co-providers and co-facilities no later than 1 business day after the request for the good faith estimate is received or after the primary item or service is scheduled, and request submission of expected charges for items or services that meet the requirements for co-providers and co-facilities. [emphases added].” This means that you are required to contact co-providers quickly to determine their potential charges.Co-provider amounts are required to be included in the Good Faith Estimate statement to the patient.Example: If you utilize functional medicine approaches in your practice and your typical patients require lab work that is billed by the lab, then the anticipated lab charges should be included in your Good Faith Estimate for the patient. GFE Required Elements and Downloadable FormThe law and rules require that the Good Faith Estimate form include very specific information. As a result, the ACS has developed an editable template for our members. Here is a full list of required elements:
- Patient name and date of birth;
- Primary service with and understandable description;
- Date of primary service;
- A full list of items or services “reasonably expected to be provided;”
- ICD-10 diagnosis codes and CPT or HCPCS codes for services (in the ACS determination, diagnosis codes would not be required until following an initial examination);
- Address, name, NPI, and TIN of each provider who will be furnishing the services;
- Other items or services that require separate scheduling and that are “expected to occur before or following the expected period of care for the primary item or service.” There must be a disclaimer directly above this list indicating that separate Good Faith Estimates will be made available (upon scheduling or request) with the appropriate details;
- A disclaimer indicating that there may be additional items or services that must be scheduled or requested separately and are not included in this good faith estimate;
- A disclaimer that the form includes only an “estimate of items or services reasonably expected to be furnished at the time of its issuance, and that actual items, services, or charges may differ from the good faith estimate;”
- A disclaimer that informs the patient of their right to initiate the patient-provider dispute resolution process if the actual billed charges are “substantially in excess of the expected charges included in the good faith estimate,” including instructions for where a patient can find information about how to initiate the patient-provider dispute resolution and that dispute process will not impact the quality of care provided; and
- A disclaimer that the good faith estimate is not a contract and does not require the patient to obtain the items or services from any of the providers or facilities identified in the good faith estimate.
Each of the above elements must be included. However, HHS does not require a specific form, as long it contains the required elements. HHS has developed a usable form, but it is multiple pages long and complex. You can find their sample form here.
The ACS has developed a shorter form that includes the elements above (except the separate scheduling portion also not included in the HHS form). Members can access that form here.
Please remember that providers must present the Good Faith Estimate in writing, but they can also present it orally. HHS has clarified that providers can satisfy the written requirement through electronic means, such as email (if requested) or a patient portal. However, they clarify that the patient MUST have the ability to “both save and print” the GFE.
Downloads
Required poster for your office
Language for your website (easy to cut and paste Word document)
Editable Sample Good Faith Estimate Form – This form has the required elements but can be edited (including adding more rows). Additionally, you can indicate a range of charges if listed services are uncertain. (Updated 1/27/2022)
Conclusion
As indicated above, these requirements are in place as of January 1, 2022, and should not be ignored or postponed. Additionally, the information in this article is based on the Interim Final Rule that was active on October 7, 2021, but could change after the comment period. Additionally, these interpretations are based on the best information currently available. Some of these requirements MAY change from future updates to the rule or based on court rulings. However, providers should implement now.
Additional Information can be found in the ChiroHealthUSA Webinar – “The No Surprises Act – What You Need to Know” hosted by Kristi Hudson and Dr. Scott Munsterman here. Download handout from the webinar.
ACS has shortened the CMS federal form and combined the state requirements of 7 AAC 86.Price and Transparency and Good Faith Estimates effective 12/20/2020 – See previous article posted – so that offices are not doing double work. The federal mandate requires that the GFE be printable so it will supersede the state option of providing a GFE “orally”. The state statute + regulations only require health care providers to provide a GFE “upon request”. The federal mandate will supersede this “upon request” only provision.
As the ACS receives more information and clarification, we will update this article and inform our members of the changes.
Thank you to Marc Abla, Executive Director, Illinois Chiropractic Society + his amazing team and Dr. Scott Munsterman with Best Practices Academy for developing the information above and making it available to the Alaska Chiropractic Society for distribution.